
Our society is being faced by a tsunami of degenerative joint disease. The incidence of this problem, particularly effecting the hip and the knee, is rising every year. Researchers are not certain as to why the incidence of degenerative joint disease is rising so sharply. Contributing factors appear to be from genetic sources, obesity and from joints that have been previously injured through trauma and athletics. This constitutes a very heterogeneous patient population that can develop degenerative joint disease.
I prefer the term “degenerative joint disease” to arthritis, as arthritis is a non-specific term indicating inflammation in a joint. Other terms for this condition are arthrosis, arthropathy, and chonromalacia. Arthritis can be caused by many factors, such as infection or inflammatory diseases like rheumatoid arthritis. Often, individuals with degenerative joint disease do not have inflamed joints, and merely have a deterioration of the joint surfaces, referred to as articular cartilage. It seems some people have an inherited vulnerability of the articular cartilage predisposing it to deterioration, and subsequent degenerative joint disease.
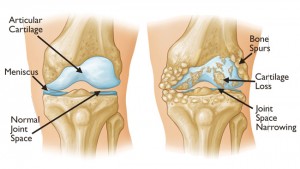
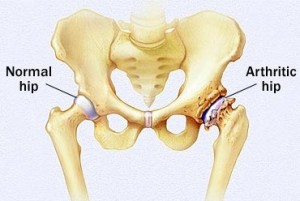
The classical manifestations of degenerative joint disease are pain and stiffness centered around a joint. There can be heat, redness and swelling of the joint. Individuals experience a phenomenon referred to as gelling where, after they have been immobile for a period of time, the damaged joint feels very stiff and painful when they first get up. After a couple of steps or a few seconds, the joint releases and they can ambulate in a more normal fashion. Individuals will often limp with degenerative joint disease of the knee or the hip. In my practice, these are the most common joints I see manifesting degenerative disease.
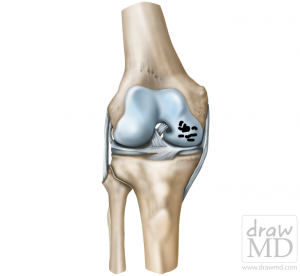
Degenerative damage to the articular cartilage of the medial femoral condyle of the knee…the first step in the process of arthritis
The diagnosis of degenerative joint disease is usually straightforward. The history is noted above. Physical examination usually reveals diminished range of motion and localized tenderness over the joint. The joint often demonstrates a specific pattern of range of motion restriction referred to as a capsular pattern. I frequently tell my patients that “hips don’t lie” and their exam usually will demonstrate whether or not they have degenerative joint disease.
The diagnosis can usually be confirmed by simple x-rays. X-rays performed in the standing position are important for the knee joint as that joint tends to wear out more in one compartment or the other. People with bowlegged knees (genu varum) will often wear out the medial compartment of their joint and people with knock knees, (genu valgum) will usually wear out the lateral compartment of the knee joint.
There is a very broad menu of management options for degenerative joint disease. Individuals should maintain as lean a body mass as possible. This minimizes the pressure on the joint and facilitates mobility. Fat cells in our body also produce inflammatory mediators, and this can make the suffering associated with degenerative joint disease worse.
Acetomeniphen often decreases joint pain and is usually the first medication recommended. Herbal preparations such as Glucosamine, Chondroitin and others have a modest effect, but the literature does not indicate that they are of tremendous benefit to most patients with degenerative joint disease.
Non-steroidal anti-inflammatory agents that can be applied topically have evidence that they are effective with little evidence of risk. This is particularly helpful for degenerative joint disease of the knee or small joints in the feet and hands. It is less useful for the hip joint.
Oral anti-inflammatory agents such as Ibuprofen, Celebrex, Naproxen and Diclofenac often help to reduce pain and stiffness with increased functional mobility. These medications have potential side effects and these need to be carefully monitored by your physician. Problems with gastrointestinal intolerance including bleeding, the kidney and cardiovascular system including hypertension and the reactivation of heart disease are known complications of using NSAIDs.
In general, people with degenerative joint disease should engage in exercises to strengthen the muscles surrounding their degenerative joint. Simple exercises such as the wall squat can increase the strength of the quadriceps, hamstrings and hip musculature and thereby help to augment shock absorption in the lower extremity and stabilize the joints. Unloading knee braces have evidence in the literature that they are helpful with asymmetric knee joint arthrosis. These can often help stabilize the joint, diminish pain and may slow the progression of the disease. They are particularly helpful when walking on unstable surfaces or trying to perform sport in the context of degenerative joint disease.
Cortisone can be injected into the knee joint and hip joint as a rescue, particularly in patients on the waiting list for joint replacement. I tend to avoid using corticosteroid injections in young people. There is evidence that corticosteroid injections lead to short term pain relief without substantial side effects. It may be surprising to learn that there are very few research papers on the long term use of steroid injections for degenerative joint disease.
Hyaluronic acid derivatives are being used more commonly and commercial names of these products are Synvisc and Durolane. They tend to have few significant side effects aside from the potential for infection at the injection site. The literature indicates that these can diminish pain and stiffness for several months after the injection. These preparations are not insured by the government, and can cost up to $400.
Newer modalities such as platelet rich plasma (PRP) are showing promise in the treatment of degenerative joint disease. This procedure entails drawing a person’s blood, centrifuging it down and obtaining a liquid rich in platelets. The platelet rich plasma is injected into the joint and can help both pain and stiffness. This is also not insured, and is even more expensive than the hyaluronic acid preparations.
One of the best operations in all of medicine is joint replacement. This is known as arthroplasty. These procedures have very high success rates, diminishing pain and increasing function in patients. In Canada, we tend to wait until people have exhausted most of the aforementioned conservative measures. The joint replacement has a finite lifespan and choosing the age at which to undergo surgery requires wisdom and discernment on both the patient’s and the surgeon’s behalf.

We have a fairly long waiting list in Canada and many patients have to wait 12 months before they can have a joint replaced after making a decision to proceed. Up to 90 % of patients have good to excellent results with hip and knee replacement surgery. The most significant risks include infection and blood clots, but these are infrequent. Most patients spend only few days in the hospital and recovery is quite rapid.

You can see that the menu of options for management of degenerative joint disease ranges from Tylenol to total joint replacement. Your pain, function and other medical conditions will determine which option is best for you.
